Abstract
Ocular graft-versus-host disease (GVHD) has the potential to lead to serious vision impairment, restriction of daily activities and deterioration of quality of life of patients after allogeneic stem cell transplantation (allo-SCT). Amniotic membrane transplantation (AMT) is an established technique in the treatment of various diseases of the ocular surface. This method could provide new options in the management of otherwise disabling severe ocular GVHD.
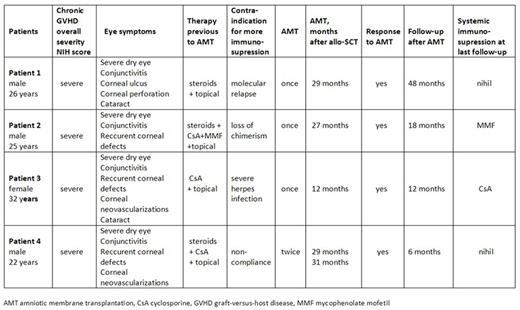
We report a case-series of four patients with severe ocular GVHD refractory to standard local and systemic therapy, successfully treated with AMT. First patient was a 26-year old male who underwent a related allo-SCT for lymphoblastic transformation of chronic myeloid leukemia (CML) and received three donor lymphocytes infusions (DLI) due to molecular relapse. Six months later he developed severe GVHD of the mouth and eye that gradually deteriorated, despite corticosteroid treatment and topical therapy, and finally led to corneal perforation. In this case AMT was used to successfully seal the corneal perforation and to avoid keratoplasty. Moreover, AMT led to a durable clinical improvement continuing for four years after the treatment without the need for systemic immunosuppression. The second patient was a 25-year old male, transplanted from an unrelated donor for a CML refractory to tyrosine kinase inhibitors, who received one DLI for mixed chimerism and consequently developed GVHD of the skin, liver, lungs and eyes. Ocular GVHD progressed despite local and triple systemic immunosuppressive treatment. In this case AMT was applied before severe corneal ulcerations developed and led to full clinical recovery. The third patient was a 32-year old female who underwent an unrelated myeloablative allo-SCT for myelofibrosis, complicated with acute liver GVHD and slow immune reconstitution. At day +150 she developed a disabling herpes keratitis and stomatitis which led to prolonged hospitalization and slow recovery. At day +280 her vision deteriorated again, this time with signs of severe ocular GVHD. We feared herpes reactivation and hesitated from increasing immunosuppression. With this rationale we decided to perform AMT which again led to significant clinical improvement. Finally, our fourth patient underwent unrelated allo-SCT in the age of 22 for high risk myelodysplastic syndrome complicated with toxic epidermal necrolysis (TEN) of the skin, mucosa and eye. In this case chronic GVHD of the eye developed eight months later and gradually progressed, partly due to patient's non-compliance with treatment. This time AMT was applied on two consecutive occasions resulting in a similarly impressive clinical effect. The latter two patients also had marked corneal vascularization possibly due to the preceding involvement of the eye with viral infection and TEN. This was efficiently treated with additional subconjunctival anti-VEGF injections. With a median follow-up of 15 months, all four patients remained clinically stable without recurrence of severe ocular GVHD.
Amniotic membrane is rich in cytokines, growth factors and protease inhibitors and serves as a biological bandage that suppresses inflammation and promotes epithelialization. In our experience, beside acute healing of corneal ulcerations in severe ocular GVHD and preventing perforation, it has a durable effect and prevents GVHD recurrence. Moreover, with the use of AMT we can avoid systemic immunosuppression and decrease both the risk of infectious complications and recurrence of the primary malignancy in allo-SCT patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.